Kidney Disease: A Global Challenge
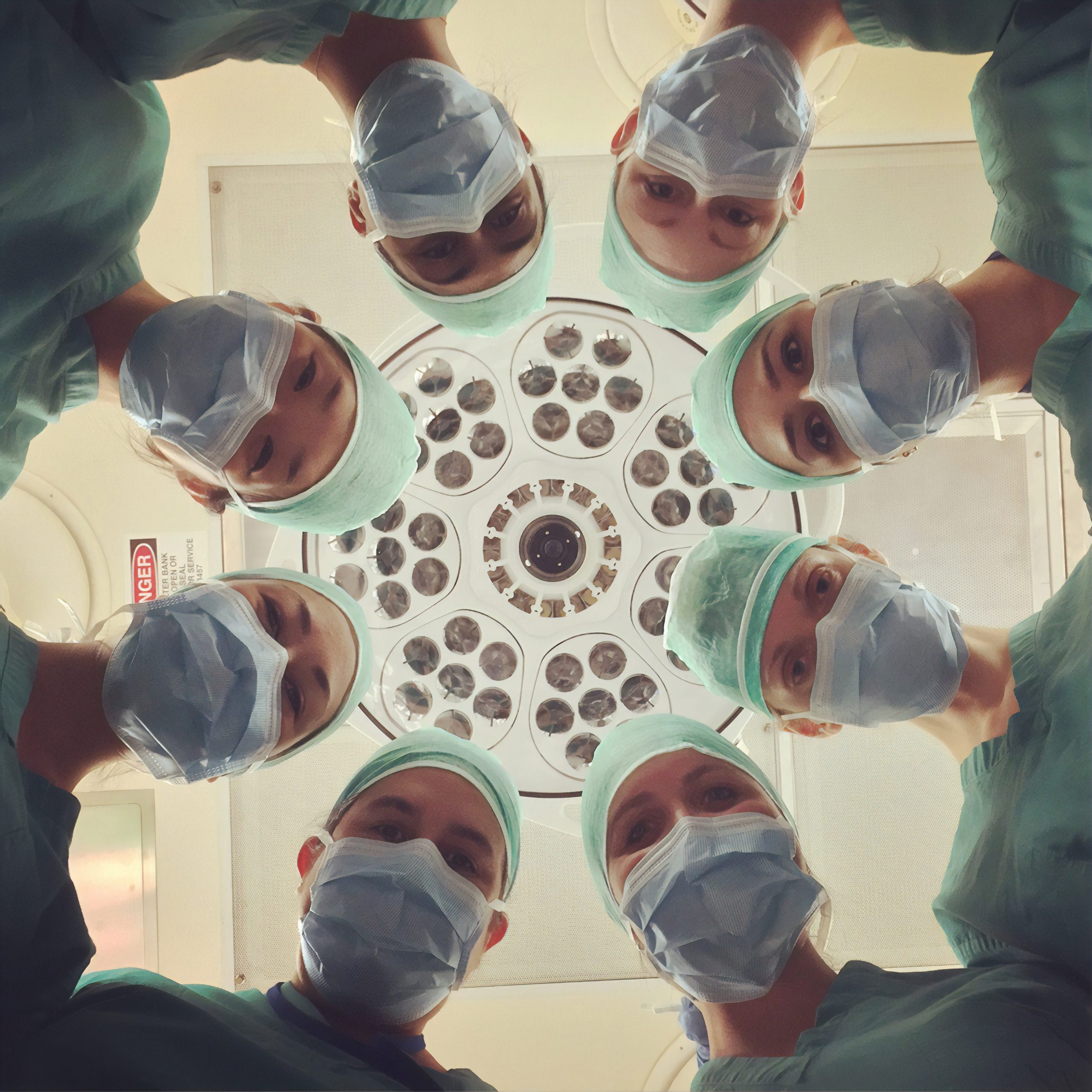
Our goal is to investigate gender-specific risk factors for the development of post-transplant malignancies (PTM) using epigenetic/genetic biomarkers in kidney transplant patients. In addition, individual diagnostics will be developed to promote personalized preventive measures. A clinical AI prognosis model and an interactive demonstrator are being developed and evaluated in clinical routine with the help of the electronic patient record. This will enable patients who carry valuable donor organs to be better protected in the long term, improve their quality of life, and reduce cost pressure on the healthcare system.
In the following, the term “gender” is used to refer to the sex assigned at birth, as retrospective data only includes this information in clinical nephrology questionnaires and it is available in the data sources. In prospective data, we will support the collection of more detailed gender-specific information.
The following are examples of gender-specific imbalances in CKD patients: Compared to men, women are up to 20% less likely to be placed on the waiting list for donor organs, despite having the same severity of disease, higher mortality during dialysis, and a similar or even better prognosis after KTx. In contrast, donor organs in living donations come more often from female than male donors, partly for gender-sociological reasons, i.e., men are more likely to receive a donor kidney from a woman than vice versa. Current studies suggest that the prevalence of CKD may be higher in women than in men, despite higher risk factors in men, such as smoking, alcohol consumption, obesity, and hypertension. Further studies suggest that the gender of the recipient patient has a significant influence on KTx outcomes, such as the risk of rejection, metabolism, and the effectiveness of immunosuppression.